A new study has revived hopes for an effective vaginal
microbicide in preventing the transmission of HIV. A
compound widely used in cosmetics and foods can block
transmission of the virus by interfering with the
immunological steps to infection,
researchers report in Nature this week.
|
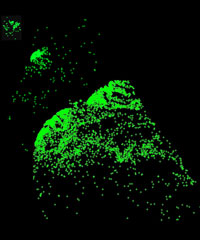
Representation of virus
expansion
after SIV exposure. Green
crosses: clusters of infected cells.
Image: A. Haase |
The compound's microbicide potential has so far been tested
in vivo only in monkeys, but in vitro results suggest it
also works against the human version of the virus.
"I think this is a really exciting study," said
Melissa Robbiani, senior scientist at the Population
Council, a New York research and policy nonprofit focused on
AIDS and reproductive health. To date, most microbicides
under development work by simply blocking the virus from
entering the body or target cells, said Robbiani, who was
not involved in the research, "whereas this is actually
targeting the immune system and modulating immune function."
With a vaccine for HIV still years away, researchers have
long pinned their hopes on a topical product that could be
applied to the vagina to stem the virus's spread. The past
few years, though, have brought dismaying results in
microbicide development. In February, 2008, a promising
microbicide gel called Carraguard
was deemed ineffective in a Phase 3 study. And the
February before that, negative results from a Phase III
trial
sank a potential microbicide called Ushercell.
Ashley
Haase at the University of Minnesota, the current
study's main author, and his colleagues began by mapping the
innate immune response initiated locally in the vagina upon
exposure to the virus. They observed growing clusters of
infected immune cells in the vaginas of monkeys exposed to
simian immunodeficiency virus (SIV), the monkey version of
HIV. First, plasmacytoid dendritic cells rushed to the
scene; those spurred a chemokine and cytokine response,
which in turn brought CD4+ T cells. The T cells would then
be infected by the virus, fueling its spread throughout the
body, Haase and coauthor
Patrick Schlievert explained in a press conference
yesterday (March 3).
The team reasoned that "if you could break one of the links
in that chain, you would break the influx of target cells
that the virus needed" to infect further cells, Haase said.
They tested the compound glycerol monolaurate (GML) in that
role because other research shows it appears to block the
growth of microorganisms such as Staphylococcus and
Chlamydia, and because it was already FDA-approved for oral
and topical use. (GML, an ester, is commonly used as an
emulsifier in cosmetics and foods such as ice cream.) In
cultured human vaginal epithelial cells exposed to HIV, they
found, GML blocked the production of molecules that appear
during inflammation and that are thought to increase
susceptibility to HIV infection.
The researchers then made up a 5% GML solution dissolved in
a lubricant called KY warming gel, and applied it to five
rhesus macaques that had been vaginally exposed to SIV. The
GML gel blocked acute infection in all five of the monkeys
tested, while four out of five control moneys, exposed to
the virus in the same way, became infected. "The results, we
think, are very encouraging," said Haase in the press
conference.
The study not only demonstrated the efficacy of GML in
blocking the virulence of immunodeficiency viruses,
Robbinani noted, but it also "provided additional evidence
for the innate response role in infection" and teased out
the roles of different immune cells in propagating the
virus. "That's important just from a biology standpoint,"
she said.
Haase and Schlievert noted that further animal testing is
needed before GML can be tested in humans. One of the five
monkeys in which the gel was tested initially appeared to be
protected from SIV, but months later developed the
infection, they said; long-term studies will have to be done
to understand how often such "occult infections" occur. "And
we also need to find much better dosing schedules [that are]
more applicable to the real world," Haase said in the press
conference.
Also, they cautioned, the compound's effectiveness in
monkeys can't be extrapolated to humans. "Vaginal
transmission by rhesus macaques is regarded by many as the
best animal model for HIV transmission, but it's still an
animal model," Haas said.
Haase et al's study isn't the only positive recent news on
the microbicide front. Last month, researchers from an
international collaboration called the Microbicide Trials
Network reported
promising results from a trial of another microbicide in
development, PRO2002, a polymer intended to interfere in
interactions between HIV and its target cells. Those
findings, from a Phase II safety and efficacy study,
prompted the Gates Foundation
to pump $100 million into the International Partnership
for Microbicides, a Maryland-based organization working on
HIV microbicide development.